Patient Info & Resources
Shared Care Policy
Shelley Manor and Holdenhurst Medical Centre
Shared Care – Policy September 2025
Shared care is a term used within the NHS to describe the situation where a specialist doctor wishes to pass some of the patient’s care, such as prescription of medication, over to their general practitioner (GP). This is something that can be requested but the guidance for all medications is that this may only be done if the GP agrees. The GP will need to consider a number of factors to decide if this is safe.
In shared care arrangements (SCAs) the prescribing Consultant or specialist team still remain responsible for parts of the patient’s care. These should be defined in the SCA and usually include any changes to the medication regime or any complications related to the medication. The presence of a specialist is also essential for the GP to be deemed to be operating under ‘shared care’. Shared care is not ‘shared’ unless it is shared by the GP with someone else.
Without this then GPs may be deemed to operating outside of Good Medical Practice. It is also important to remember that formal shared care arrangements are voluntary on the part of the GP and the GP should be mindful of their own clinical competence and workload capacity when considering agreeing to enter into such an arrangement. Workload requested for an
individual patients will need to be considered in balance with the reasonable needs of the practice population and whether further workload can be absorbed by the practice team safely.
Shelley Manor & Holdenhurst Medical Centre will consider the following points and will not take on prescribing from any NHS provider if the practice is not satisfied that these requirements can be met.
• The specialist has sought agreement of the GP and made clear the nature and responsibilities of each party of the shared care arrangement before transferring any care or prescribing and you feel assured by what you have seen
• Do you feel that the prescribing and associated knowledge required falls within the scope of your team’s professional competence?
• Do you feel this falls within your team’s workload capacity?
• Are there adequate resources and sufficient capacity for the work of managing safe systems for monitoring and prescribing for this medication in your practice? For NHS providers, are they locally commissioned or have they been approved by your ICB as
working in line with UK best practice and local prescribing guidelines/shared care protocols?
• For private providers are you satisfied that the provider is appropriately accredited, practicing in line with UK best practice and will prescribe and monitor patients in line with locally agreed pathways apply?
• For those under private providers – Has there been an agreement with the patient that prescribing will cease, if the patient for whatever reason, is unable to continue follow up with a private provider?
• SMHMC will not prescribe ‘Red’ medications (as outlined on the Dorset Formulary) requested or initiated by private providers at all.
PATIENT NEWSLETTER
SMH Patient newsletter April 2025.pdf
(Download our latest newsletter here - lots of useful info included)
PRESCRIBING DIAZEPAM AND FEAR OF FLYING POLICY
Bournemouth East Collaborative Primary Care Network (Shelly Manor and Holdenhurst Medical Centre, Beaufort Road Surgery, Southbourne Surgery and Littledown Surgery) does not issue sedatives such as diazepam for fear of flying. This policy decision has been made by the GP Partners and is adhered to by all prescribers working in the practice.
We appreciate that fear of flying is very real and very frightening. One way to tackle this is to attend a Fear of Flying course run by the airlines and we have listed a number of these below:
- EasyJet – 02038131644
- British Airways – 01252793250
- Virgin Airways – 01423714900
Alternatively, if you still feel you wish to have this medication prescribed then you would need to see a doctor with Aviation training. These are usually private.
Why Diazepam is not recommended:
- Diazepam is a sedative, which means it makes you sleepy, more relaxed and can significantly delay your reaction times. If there is an emergency during the flight it may impair your ability to concentrate, follow instructions and react to the situation. This could have serious safety consequences for you and those around you.
- Sedative drugs can make you fall asleep, however when you do sleep it is an unnatural (non-REM) sleep. This means you won’t move around as much as during natural sleep. This can cause you to be at increased risk of developing a blood clot (DVT) in the leg or even the lung. Blood clots are very dangerous and can even prove fatal. This risk is even greater if your flight is greater than four hours.
- Whilst most people find sedative medications like diazepam have a relaxing effect, a small number of people can feel more agitated or even aggressive after taking it. Diazepam can also cause disinhibition and lead you to behave in a way that you would not normally. This could impact on your safety as well as that of other passengers and could also get you into trouble with the law.
- Benzodiazepines are not licensed for use in phobias. They are potentially very addictive, and dependence can form quickly.
- Diazepam and similar drugs are illegal in several countries. They may be confiscated, or you may find yourself in trouble with the police if you are carrying any on arrival.
Please also note that following the same advice above we are not encouraging the use of diazepam for dental appointments, hospital scans or other procedures.
Date approved: 14/12/2023.
Written by: Stuart Robinson (Lead Clinical Pharmacist for the PCN)
We're always looking at ways we can help patients.
On this page you can find some of the resources and services we offer, as well as being able to learn more about the partners we collaborate with.
Services
- District Nurses & Health Visitors
- e-Referrals
- Local Services & Activities
- Mental Health
- Midwives
- Musculoskeletal (MSK) Practitioner Service
- Worried about losing your home?
- Cancer information and support
If you or someone you care about has been diagnosed with cancer, please see the links below for support available to you.
- Macmillan
- Cancer Care Map
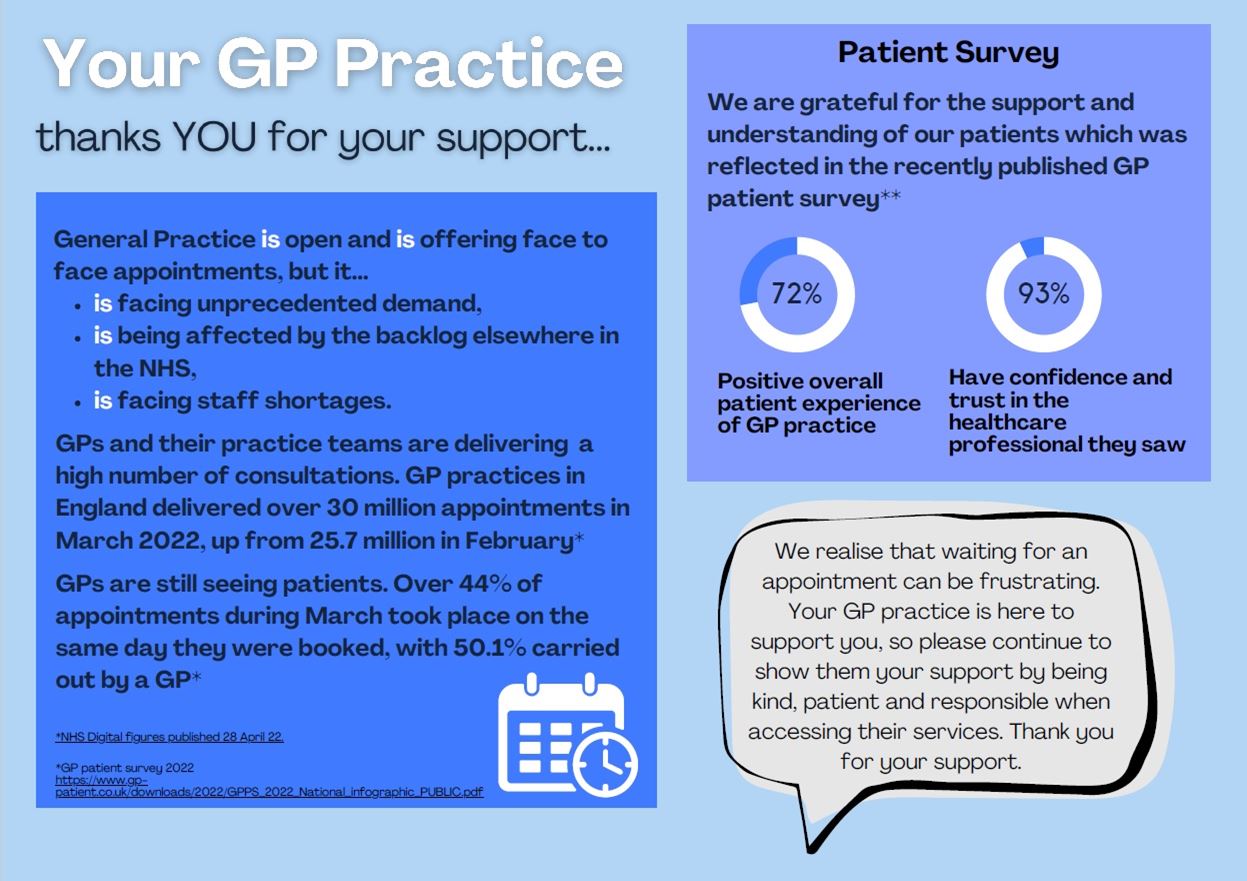
In July our Doctors saw 1788 patients in face to face appointments.
We had a total of 483 patients not attending their appointments with any of our healthcare professionals, 176 of those were GP appointments.
Just under 10% of our total Face-to-face GP appointments have been wasted. Please let us know if you can not attend as it just makes the wait to see a GP even longer for other patients.
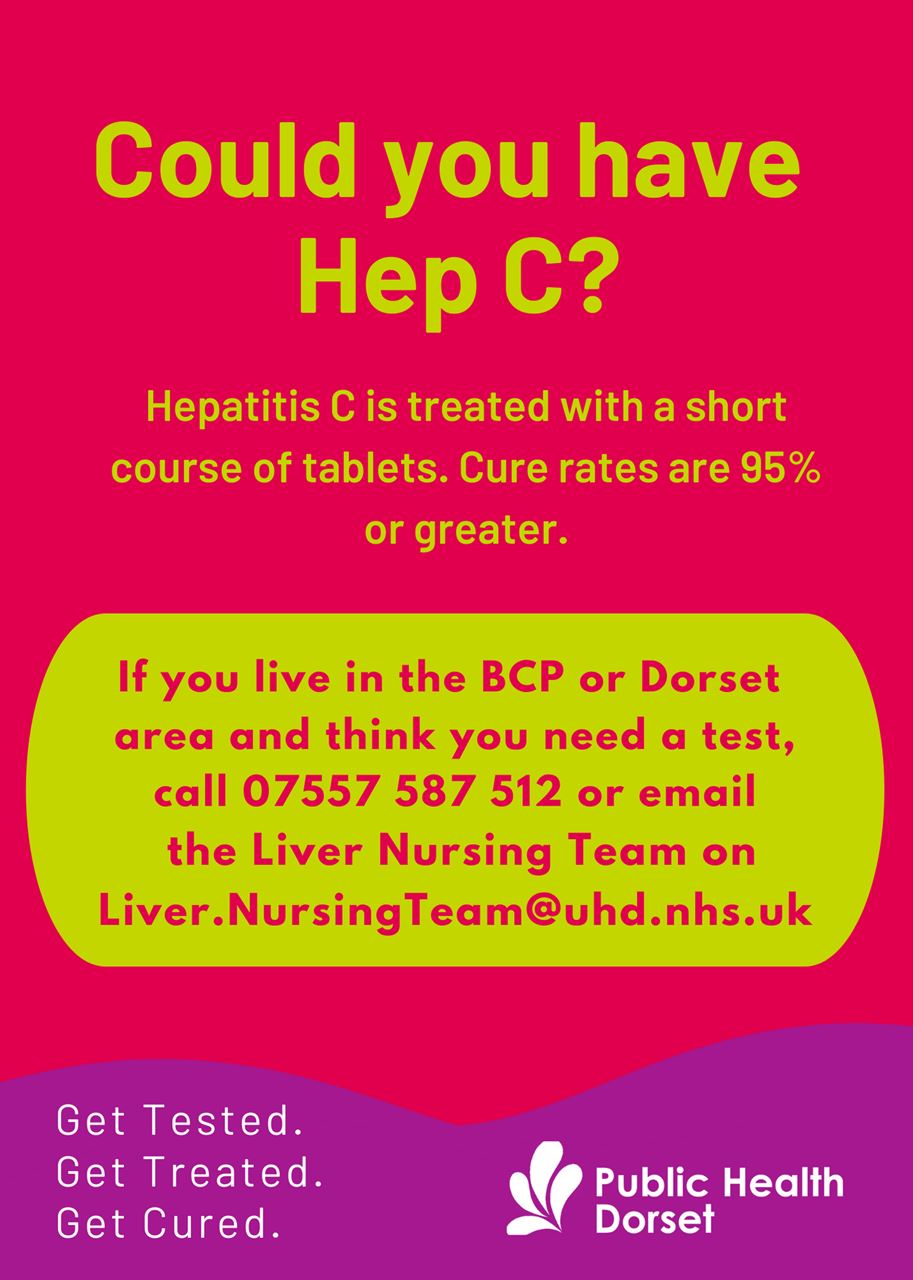
What is Hep C
-
Hepatitis C, or Hep C, is a virus spread through exposure to infected blood.
-
Hep C most commonly affects the liver and can cause serious damage without you knowing – 50 per cent of people living with Hep C don’t know they have it.
-
If left untreated, Hep C may cause potentially life-threatening damage to the liver and may also have adverse effects on the digestive system, lymphatic system, immune system and brain.
Are you at risk?
Are you or your client/patient at risk? Hepatitis C is usually spread through blood-to-blood contact.
Risks for contracting the virus include:
-
Having a blood transfusion or organ transplant before 1992
-
Using recreational drugs that involve needles or straws
-
Having medical, dental or cosmetic procedures (including vaccination) using unsterilised equipment
-
Using unsterilized tattoo or piercing equipment
-
Sharing personal items such as razors or toothbrushes
-
Engaging in sexual contact with a person infected with Hep C
-
Having spent time in South Asia and particularly India, Pakistan and Bangladesh
Take the Hepatitis Trust quiz to find out if you are at risk of infection http://hepctrust.org.uk/quiz
Testing and Treatment
-
Don’t be misinformed, Hep C treatment has changed a lot over the years.
-
A simple finger prick test will tell you if you have it and treatment is usually a course of tablets between 8 to 16 weeks long with very few side effects.
-
Testing has never been easier so why wait?
-
Take action, get tested, get treated, get cured.
-
For more information or to book a simple test contact 07557 587 512 or email the Liver Nursing Team on Liver.NursingTeam@uhd.nhs.uk/
Page created: 14 May 2021